INDEPENDENT MEDICAL REPORT BY DR. JOHN MONAGHAN, WORLD-LEADING GYNAECOLOGIST, INTO THE CARE PROVIDED TO MAUREEN DESMOND AT THE MATER HOSPITAL CITES NEGLIGENCE AND FAILURES IN DUTY OF CARE
Please note that this report was submitted by Stephen Desmond to the Inquest into Maureen Desmond's death conducted by The Dublin City Coroner, and as such is part of the public record of this inquest--and it is provided here as part of that public inquest record.
MEDICAL REPORT
Prepared by
Mr J M Monaghan, M.B, FRCS(Ed)., FRCOG
Consultant Gynaecological Surgeon
in the matter
of
Mrs Maureen Desmond
Date of Birth: 26.06.1937
Date of Death: 04.09.2011
Requested by
David Harris, Solicitor.
Ivor Fitzpatrick & Company,
44-45 St Stephen’s Green,
Dublin 2,
Ireland
22nd August 2013
John M Monaghan MB, FRCS(Ed), FRCOG
SUMMARY CV
My name is Mr. John M Monaghan, Consultant Gynaecological Oncologist; I was Director of Gynaecological Oncology Services at the Regional Department of Gynaecological Oncology at the Queen Elizabeth Hospital at Gateshead, 1978 – 1999. I was a Senior Lecturer in Gynaecological Oncology at the University of Newcastle upon Tyne and had been in this post for 28 years until I retired in June 2002.
I have published extensively on all aspects of Gynaecological Oncology, and have written over 42 chapters and text books on Gynaecological Oncology subjects and recently have published with Professor Albert Singer a text book on Colposcopy, Lower Genital Tract Precancer, an Atlas of Colposcopy (First and Second Editions), and also Co-Editor with John Shepherd of Clinical Gynaecological Oncology, First and Second Edition. I have edited Bonney's Gynaecological Surgery, Ninth and Tenth editions. Eleventh edition published February 2011. I am co-editor of 'An Atlas of Gynaecological Oncology', first and second editions, third edition published May 2011. It has now been commended in the BMA Book Awards 2012.
I have carried out a wide range of surgical and gynaecological oncology procedures over 28 years. During the 1990's I extended my laparoscopic experience, which began in 1968, into the area of advanced minimal access surgery, now having an extremely large experience of laparoscopic assisted vaginal hysterectomy and the wide range of radical laparoscopic procedures in gynaecological oncology. I have written extensively and lectured on gynaecological surgery in all its forms around the world.
I was a founding member of the British Gynaecological Cancer Society and held a number of offices as well as being a Council member for some years. I was a founding member of the International Gynaecological Cancer Society and have been Membership Secretary, a member of Council, and Vice-President. I am an honorary member of the Felix Rutledge Society, Member of Society of Pelvic Surgeons and Member of Society of Gynaecological Oncologists, all U.S. Societies.
I was appointed the RCOG Sims Black Visiting Professor for the year 2001 to visit the Far East. I was appointed Lead Clinician for the National Cancer Services Collaborative, Modernisation Agency, 2001.
In June 2002 I retired from Clinical work in the NHS but continued as National Clinical Lead for the Cancer Services Collaborative until June 2003. In 2003 I was registered with the Italian Medical Council and have been teaching surgery and setting up Multidisciplinary Treatment programmes in Emilia Romagna until September 2004.
GMC Registered Number: 0551609
MDU Number: 075565E
I am asked by David Harris Solicitor to prepare a report in the matter of Mrs Maureen Desmond - Date of Birth: 26.06.1937 concerning her care at Mater Hospital Dublin. I understand my overriding duty in writing this report is to assist the Court on matters which are within my expertise and I also understand that this duty overrides any obligation to David Harris (Solicitors) or their client.
I understand that my overriding duty in writing this report is to assist the court on matters within my expertise and that this duty overrides any obligation to David Harris, Solicitor or their clients. I confirm that I have complied with that duty and will continue to do so and that I am aware of the requirements set out in Part 35 of the Civil Procedure Rules and the accompanying Practice Direction, the Protocol for Instruction of Experts to give evidence in Civil Claims and the relevant Pre-action Practice Direction/Protocol.
I confirm that I have made clear which facts and matters referred to in this report are within my own knowledge and which are not. Those that are within my own knowledge I confirm to be true. The opinions I have expressed represent my true and complete professional opinions on the matters to which they refer.
22nd August 2013
MEDICAL REPORT
Documentation
I have available to me:
1 A detailed chronology prepared by Mr Stephen Desmond to include Mater Gynaecology notes, Letters of Complaint to the Mater Hospital, The General Medical Council Ireland, Letters from Mr W Boyd, A summary report from [The] London Clinic.
2 Records of the final hospital admission under Dr Lambert and Medical Oncology records.
History and Chronology.
1.Mrs Maureen Desmond was a healthy lady of seventy when in November 2007 she was referred by her GP to the Mater Hospital rapid access clinic because she was complaining of abdominal discomfort and a clear profuse vaginal discharge. At the clinic visit on the 8th of November 2007 a CT scan was organised after examination had not revealed any significant findings apart from a large incisional hernia in the abdominal wall. The CT scan result showed an enlarged uterus and an endometrial thickness of 14 mm, described as heterogenous in the report; (an acceptable upper limit for the endometrium in a seventy year old is approximately 4 mm). An Ultra sound scan was then organised which confirmed the enlargement of the uterus and the endometrial thickness was identified as 13.7 mm. Again described as heterogenous. The ovaries were described as normal.
Comment; Such a finding in a post menopausal patient should generate an appointment within two weeks of the GP letter
3 Mrs Desmond and her son were alerted by the ultrasonographer to the importance of dealing with this situation and she was immediately referred to a gynaecologist, Mr William Boyd at the Mater hospital. In spite of the importance of the findings there was a large delay in achieving this first consultation which took place in 9th of April 2008. The letter written by Mr Boyd dated the 9th of April 2008 to the GP Dr Mary Chambers states the findings of the scans and notes the thickened endometrium and recommends a hysteroscopy and D&C. He Notes that she is 70 and diabetic and will need a pre-operative assessment.
4 Comment; the approach recommended is standard and should be instituted within two to four weeks of this consultation. In fact after prompting by the family an arrangement for an out patient hysteroscopy and Pipelle sample was made for 13th of August 2008. This is some nine months after the original referral and the worrying changes identified on the CT Scan and the ultra sound scan.
5 The procedure of Outpatient Hysteroscopy and Pipelle sample was carried out by Dr Moses on the 13th of August. The operation note is available and reads as ‘Hysteroscopy’
Under description of operation Dr Moses writes C/O Thickened endometrium on USS, No Symptoms.
O/E Abd Soft, NE N(ringed), size of A/V uterus. ( this means a normal sized uterus leaning forwards) Adnexae NAD, (this means ovaries and tubes were normal). Cx ….. ( not decipherable).
Hysteroscopy- moderate view.
N (ringed) Cavity. (means normal cavity)
L ostia seen, (the hole at the cornua of the uterus seen)
R ostia NAD ( I am not sure why a different comment is made here)
No Lesion.
Pipelle attempted, no sample as atrophic cavity.
Please discharge TCI, ( to come in ), if pv (per vagina) bleeding
Signed Moses
6 It is quite alarming that Dr Moses appears to be willing to ignore the findings of a CT Scan and an Ultra sound Scan and rely on what is clearly an unsatisfactory procedure where he has failed to identify an enlarged uterus, has mistaken a markedly thickened endometrium for an atrophic one and having in his own words ‘attempted’ a pipelle sample and failed. His decision to discharge the patient in the face of significant worrying findings is in my view so substandard as to be negligent.
7 At the very least a review of the patient should be arranged and a formal Hysteroscopy and D&C as advised by Mr Boyd should be carried out. The Pipelle sampler relies on suction to draw in a sample of endometrium into its cavity which is removed as the sampler is withdrawn. If the clinician does not perform the procedure correctly no sample will be produced. It is unacceptable to presume that because no sample has been obtained that the endometrium must be atrophic. This is particularly so when there is evidence on two different scans that there is marked thickening of the endometrium. It is clear in the light of subsequent developments that Dr Moses performed duties in an incompetent manner, including mis-assessing the size of the uterus at initial examination.
8. Sadly the news that there was no problem was received by Mrs Desmond and her son and no further action took place until Mrs Desmond began to bleed vaginally and was referred back to the hospital where seen by Mr Boyd in July 2010 when Hysteroscopy and D&C performed under general anaesthetic revealed an obvious cancer of the uterine cavity. The procedure which should have been done some two years previously was performed under general anaesthetic without any problem. A high grade papillary serous endometrial cancer was identified. Later on the 22nd of July 2010 a fine needle aspiration of an ‘omental node’, was taken which showed infiltration with the same cancer, that is the cancer had spread to the peritoneal cavity and was inoperable. A CT Scan confirmed abdominal disease at this time.
9.On the 22nd of December a PET Scan confirmed residual disease in the uterus and in the abdominal cavity. Curiously in a letter dated 15th of December 2010 Mr Boyd wrote to Dr Noeleen Gleeson a consultant gynaecologist at the St James’ Hospital Dublin asking for a second opinion. He notes that Mrs Desmond had had symptoms of discharge and had a hysteroscopy ‘but unfortunately did not have a D&C at the time’. Mr Boyd somewhat disingenuously does not mention that this missed opportunity was some two years before the eventual diagnosis. He then goes on to describe an ‘ovarian cancer’ which had been treated with three cycles of chemotherapy but with little response. This is not borne out by the scans which show a 25% reduction. He asks Dr Gleeson to consider surgery as an interval procedure.
10. Comment; There seems to have been some curious changes in opinions about the fitness or other wise of Mrs Desmond to survive surgery. One minute she is too unfit for a Hysteroscopy and D&C and next has a Hysteroscopy and D&C and now is being considered for extensive debulking surgery.
11. On the 3rd of December 2010 Mrs Desmond GP Dr Chambers writes to Medical records at the Mater Hospital asking if she could have a copy of the letter and notes relating to the admission of 13.08.08
12.Attempts were made to treat Mrs Desmond with chemotherapy but she had adverse reactions including Staphylococcal infection in her port and possible excessive dosage of chemotherapeutic agents. These problems are the subject of a separate complaint from Mr Stephen Desmond. These complications resulted in prolonged hospitalisation. No further action took place in terms of active treatment and Mrs Desmond was looked after by the palliative care team who seemed to labour under the misapprehension that the patient had an ovarian cancer.
13. Eventually Mrs Desmond was admitted to hospital through A&E To the Mater hospital with shortage of breath. She died of a pulmonary embolus on the 4th of September 2011. Her care in this last episode is the subject of a separate complaint from Mr Stephen Desmond.
14. A Coroner’s post mortem was carried out which confirmed the cause of death to be a Pulmonary embolus secondary to metastatic endometrial adenocarcinoma. Both ovaries were described as normal by the pathologist.
15.Mr Stephen Desmond has made representations to the General Medical council concerning the standard of care given to his mother by Mr Boyd, Dr Lambert and Professor McCaffrey.
Summary. Any woman aged 70 presenting to her doctor with a significant new discharge from the vagina whether accompanied by bleeding or not should be treated as an urgent and concerning case. The initial care of Mrs Desmond was correct as an Ultrasound of the pelvis and CT scan was organised. The ultrasound is the diagnostic tool of choice in these circumstances and it showed an endometrium 13.7 mm thick demonstrating heterogenous patterns. This report quite rightly rang alarm bells and an appointment was made to see a gynaecologist, ( Mr W Boyd)
The gynaecologist was also stimulated by the unusual and concerning findings on the ultrasound and CT Scan to organise a Hysteroscopy and a D&C.. This procedure should have been performed as a matter of urgency within the next four weeks. For whatever reason Mrs Desmond was not brought in for the procedure until nine months later. This is not acceptable practice and is negligent
The procedure was also translated into an Outpatient Hysteroscopy and Pipelle sample. Such a procedure is often very difficult for the doctor and uncomfortable for the patient. The procedure was also done by a junior doctor. This would have been acceptable if that person had been supervised and his/her findings checked. From Mr Desmond’s communication to me it would appear that there was difficulty in visualising the screen due to incident light and the junior doctor made the diagnosis of an atrophic endometrium and no Pipelle sample was obtained. In the operation record Dr Moses records that a ‘Pipelle sample was attempted’.
Mr Desmond was then discharged from the clinic without a diagnosis, without any explanation for the conflicting findings on Ultrasound/CT Scan and hysteroscopy, and without any arrangement for review to either resolve this conflict or to identify other investigation or to proceed to the original proposed Hysteroscopy and D&C.
In the event two years later the patient was identified with inoperable uterine cancer and died one year thereafter..
Comment.
The initial phases of this case were well managed.
1/. The Ultrasound and CT scans were appropriate investigations.
2/. Once an abnormality had been identified in the endometrium referral to a gynaecologist was correct and the organisation of a Hysteroscopy and D&C was correct.
To perform the procedure some nine months later was unacceptable and negligent.
3/.Changing the procedure to an outpatient Hysteroscopy and Pipelle sample was acceptable so long as a good view of the interior of the uterus could be seen and a confident Pipelle sample produced. In these circumstances of an ‘unsatisfactory test’. A move to a formal Hysteroscopy and D&C under anaesthetic was mandatory. Not to do so is substandard and negligent
4/. If a further procedure had not been organised a review of the case should have been performed to determine why there was a discrepancy between the ultrasound/CT Scan result and the findings at Hysteroscopy. Not to do so is substandard and negligent. A repetition of the ultrasound would have been a minimal requirement.
5/. To discharge the patient without any review of either the case or the patient is substandard and negligent.
6/. In my view there was clear evidence of a breach of duty of care in this case. In causation terms, if Mrs Desmond had had a diagnosis of her uterine cancer made some one year and eight months prior to its eventual diagnosis she would have had a simple procedure such as a total hysterectomy with removal of ovaries and on the balance of probabilities would have been cured of her cancer. Uterine cancer has a very high cure rate when the cancer is diagnosed within the confines of the uterus but the cure rates drop rapidly when spread has occurred outside the uterus. It is a pity that the opportunity to diagnose this cancer at an eminently curable phase was lost due to the failings of the Mater Hospital and its staff .
Statement of Truth
I confirm that I have made clear which facts and matters referred to in this report are within my own knowledge and which are not. Those that are within my own knowledge I confirm to be true. The opinions I have expressed represent my true and complete professional opinions on the matters to which they refer.
Signed ………………………….
J M Monaghan
Date: 22nd August 2013
*****************************************************************************
FURTHER MEDICAL REPORTS
1) 13th January 2014: The Coroner's review of Maureen Desmond's Radiology which confirms a Stage I pathology when Maureen was discharged from The Mater without a biopsy in August 2008, and cancer on the CT scan of June 2009 which was read at The Mater as "normal"
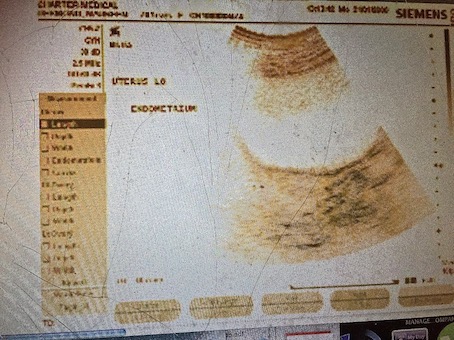
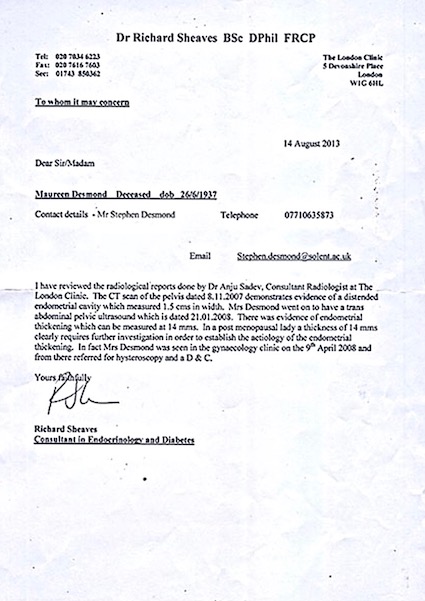
The reports below were written by Charter Medical Dublin and The London Clinic on Harley Street. Charter Medical reviewed their original scans on Maureen of January 2008---Charter Medical confirmed and have stood over their original findings, i.e. a 14mm thickened endometrium, abnormal distended uterine cavity, and enlarged uterus. The London Clinic also reviewed the original scans and reports, fully agreed with Charter Medical, and confirmed an endometrial thickening of 14mm, distended uterine cavity, etc. According to Dr. Monaghan's expert report, these findings on the original scans contradict the finding made by The Mater's Gynaecology Registrar when he discharged Maureen from The Mater Gynaecology Clinic after hysteroscopy and without a biopsy in August 2008. The Gynaecology Registrar at The Mater wrote that he could not obtain a biopsy sample because of endometrial atrophy (an ultra thin lining of the endometrium)--However, a frame (immediately below) from the original ultrasound in question does NOT show atrophy--it shows a gross thickening of the endometrium, according to Charter Medical and The London Clinic.
There is no explanation as to how The Mater's Gynaecology Registrar mistook (according to Dr. Monaghan), on hysteroscopic view, a grossly thickened 14mm endometrium for an ultra-thin atrophic endometrium, other than the evidence given by Maureen's son to the inquest into her death. At the inquest Maureen Desmond's son stated that he was present outside the examination room when The Mater's Gynaecology Registrar performed the hysteroscopy and Stephen heard the nurse saying to him "Doctor, we can't see the screen...will I pull the blind". Stephen Desmond then testified that The Mater's Gynaecology Registrar replied "No".